In the CY 2026 Home Health Final Rule, CMS updated how functional impairment levels are calculated under PDGM. Each home health episode is assigned a functional impairment score based on responses to OASIS Functional items (commonly called M-items), which assess a patient’s ability to perform activities of daily living. These scores directly influence case‑mix and payment rates.
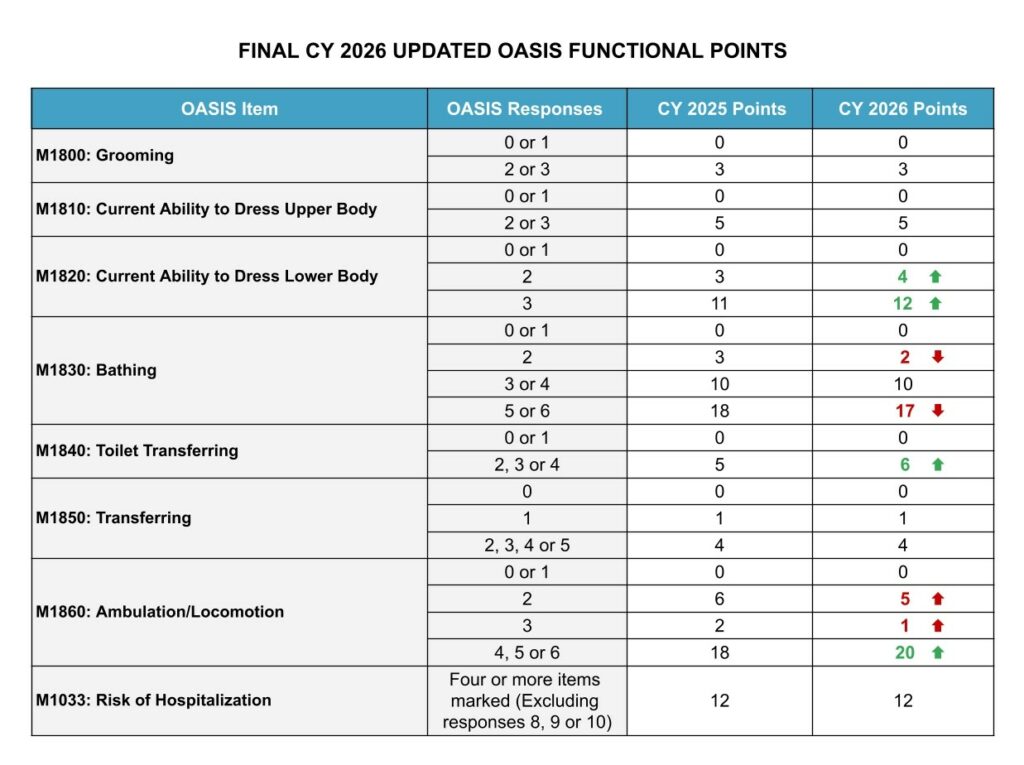
For CY 2026, CMS recalibrated the functional points using recent claims data to better reflect current patient needs and resource use. Responses to the M-items now carry revised point values, outlined in the table below. The sum of these points determines low, medium, or high functional impairment levels, which guide PDGM payment adjustments.
Accurate scoring of the M-items is critical. Over- or underassessment of functional abilities can result in misaligned payments, inadequate resource allocation, and potential compliance risks. Regular clinician education is essential to maintain scoring accuracy. In addition, leverage your QA processes to ensure proper interpretation of patient functional ability and verify that all responses align with clinical documentation. These steps not only protect agency revenue but also support high-quality patient care by ensuring that patient needs are accurately captured and addressed.

