*In the interest of client confidentiality, the agency name was changed for this case study.
Using efficient coding and OASIS documentation solutions, Endeavor Home Care optimized its reimbursement levels and improved the performance of its clinicians with the help of Qavalo.
Qavalo’s expert coders were able to capture all diagnosis codes deduced from medical records in successful collaboration with Endeavor’s in-house team. Meanwhile, Qavalo’s comprehensive quality assurance (QA) program not only improved the OASIS M item scoring, but also helped clinicians better their patient assessment skills.
Benefits Realized
- Higher reimbursement values from comorbidity adjustment
- Higher reimbursement values from the OASIS M item data (Functional Impairment Level)
- Successful collaboration between the in-house team and outsourced team
- Improved clinician-patient assessment skills
- Areas that need further improvement are identified
Challenges in Coding and OASIS Documentation
Diagnosis coding and functional M items or activities of daily living (ADL) data are two (2) significant areas that can be reinforced to optimize reimbursements. These two factors create a significant impact under the Patient-Driven Groupings Model (PDGM), not only in the calculation of the case-mix weight and reimbursement, but also in helping to support the medical necessity of the care to be provided to the patient in the documentation. Let us take a closer look at the elements that affect these two factors.
Comorbidity Adjustments
There are four (4) steps in the grouping of a patient into the PDGM Home Health Resource Group (HHRG), which establishes the case-mix weight and eventual payment. ICD-10 coding makes up 50% of that process.
While the primary diagnosis (from the claim) of the patient is the sole determinant of the Clinical Grouping of the patient, the comorbidity adjustment is based on the secondary or other diagnoses that are found on the claim. The comorbidity adjustment has three levels:
- No Comorbidity Adjustment – No secondary codes meet criteria for higher resource use.
- Low Comorbidity Adjustment – Only one secondary code meets the criteria for higher resource use.
- High Comorbidity Adjustment – Two or more secondary codes meet the criteria for higher resource use.
The case-mix weight is increased by 6.01% with a Low Comorbidity adjustment and an additional 12.95% if a High Comorbidity adjustment applies.
Often, comorbidities are not clearly outlined in the documentation received from the referral source. In some cases, only symptom codes or ‘R Codes’ (which are symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified) are indicated in the documentation; these are not allowed to be assigned as secondary diagnosis.
Functional Impairment Level
The functional impairment level is based on the responses to eight (8) OASIS-D1 items for ADL. The responses from all M items based on a point system determine the functional impairment level depending on the clinical category.
The Centers for Medicare & Medicaid Services (CMS) looks at the above OASIS assessment items and related resource usage over a 30-day period and assigns a point value to each item.
Points reflect relative resource use. OASIS item responses that indicate higher functional impairment and a higher risk of hospitalization are assigned higher points. OASIS points are then summed up to determine an overall functional score. After, this score is compared with the PDGM clinical grouping thresholds to determine whether the 30-day period is assigned a low, medium, or high functional impairment level.
The accuracy of responses to the M items relies on the clinicians’ judgment and their patient assessment skills, which is often a challenge due to the complexity of M items. Each one involves different time considerations and requires different levels of assessment for different aspects of a patient’s ability to perform activities.
The Qavalo Method
To help address the above challenges and improve reimbursement levels, the following coding and QA review solutions are applied by Qavalo:
- Accurate diagnosis sequencing
- Proactive query for additional information for coding
- Comprehensive QA review with focus on the M items
- Supporting of reeducation of clinicians
- Efficient OASIS review for accurate M item scoring
Let us take a closer look at the impact of Qavalo’s solutions in numbers using claims data from e Endeavor from May to June 2021:
Expert and Proactive Coding
Out of 250 charts coded, 79 or 32% realized an increase in reimbursement value after secondary diagnoses have been assigned.

For the 79 charts, secondary diagnoses triggered a comorbidity adjustment which increased the total reimbursement value by 6%.
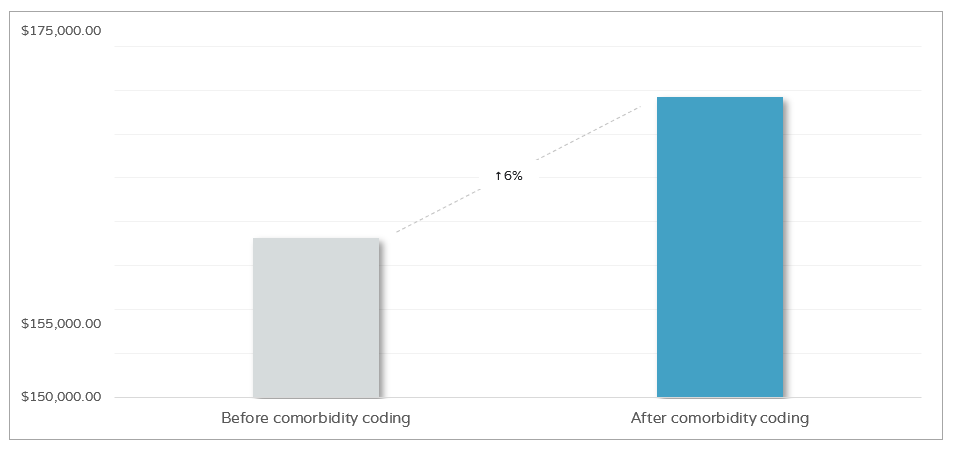
The positive results prove how Qavalo’s team of coders are well accustomed to coding conventions and guidelines, medical terminologies, and disease processes. To ensure all comorbidities are captured, Qavalo coders thoroughly analyze all relevant patient medical records, such as history and physical (H&P) examination, discharge summaries, operative reports, and progress notes.
Furthermore, Qavalo coders coordinate queries to in-house teams about missing information in the documentation that can substantiate coding assignments. The in-house team, especially the intake team, communicates these queries to referral sources so they can then provide the necessary information.
Accurate Functional M Item Scoring through OASIS QA Review
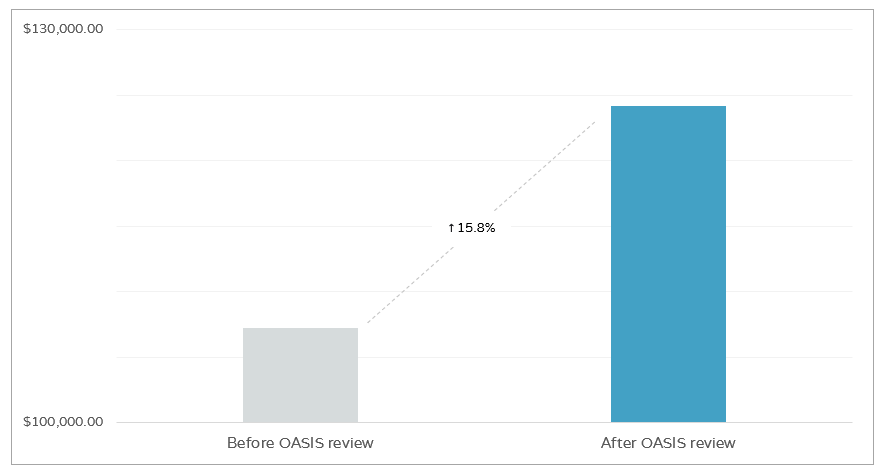
Out of 250 charts reviewed from May to June 2021, 22% had an increase in the reimbursement level. By analyzing the patient assessments, QA reviewers found more opportunities to improve the M item scoring, which resulted in an increase in the reimbursement level.

It can also be noted that after OASIS review, 11% of the charts had a decrease in its initially coded reimbursement value. Comprehensive QA review caught inconsistencies in some functional M item documentation which had to be corrected in order to accurately reflect the patient’s condition in compliance with CMS standards.
Nonetheless, a 15.8% increase in the reimbursement value was realized for 22% of the charts after OASIS M item scoring was improved.
On the other hand, we also recognized that a considerable number of charts did not have any change in the functional impairment level (or reimbursement amount per se) even after the OASIS QA review. This is because Endeavor clinicians have improved in patient assessment and learned to accurately score the M items through continued education from the QA program. This is evident in the declining number of QA points flagged for the OASIS M items during the QA review.
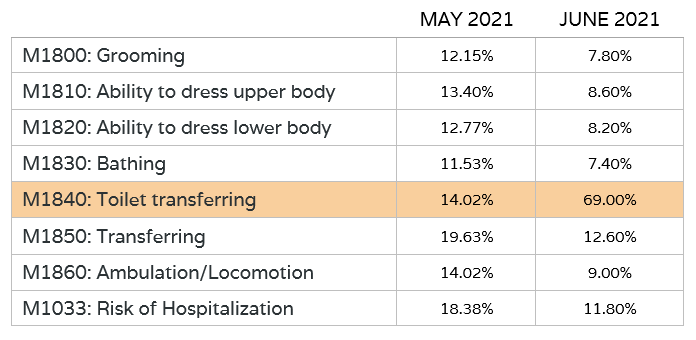
The data shows that on most M items, the rate of revisions continued to drop despite the increase in total number of charts reviewed. This signifies the improved accuracy of clinicians’ scoring of the M items.
Moreover, leveraging on data insights from Qavalo, Endeavor was also able to identify their clinicians’ areas of improvement. Table 2.3 also shows that clinicians may have challenges responding to M1840: Toilet transferring. This is evident in the significant increase in the rate of revision on the said area. Therefore, this can then be Endeavor’s focus for further clinician education and process improvement.
Targeting Areas of Concern with Precision
As reflected in the data, Endeavor improved their reimbursement levels by optimizing their HHRG through the help of accurate coding and efficient OASIS QA review. In addition, proactive and knowledgeable coders maintained effective collaboration with the in-house team to secure substantial documentation and to find opportunities to optimize code assignment. A sustainable QA program also supported clinician reeducation through the use of data analytics to target areas of improvement in clinicians’ patient assessment and OASIS documentation skills. Continued implementation of these best practices and effective solutions will lead to lucrative progress in many aspects of the home health business.

