Similar to the risks of failing to sign a legal document, home health documentation signatures are critical as it validates the healthcare services received by patients.
The purpose of a practitioner’s signature in patients’ medical records and other important documents is to demonstrate that services submitted to Medicare have been accurately and fully documented, reviewed, and authenticated. Furthermore, it confirms that the physician or non-physician practitioners (NPPs) have certified the medical necessity for the services submitted to the Medicare program for payment consideration.
Needless to say, signatures must be legible and should include the practitioner’s first and last name. It is also recommended to include applicable credentials (e.g. P.A., D.O., or M.D.). On top of that, there are certain guidelines that agencies can follow to make sure signatures are acceptable based on standards by the Centers for Medicare & Medicaid Services (CMS).
Signature Requirements
Here is a checklist to ensure a signature’s validity:
- Services provided or ordered must be authenticated by the author.
- The signatures shall be handwritten or electronic.
- The signature must be legible.
- The signature must include the credentials of the individual and be dated.
- Medical record entries completed by a scribe must be authenticated by the treating physician or NPP’s signature and date.
Let us look at different scenarios:
- Dated Signature
All signatures need to be dated and timed. However, Medical Review (MR) must be able to determine on which date the service was performed or ordered. If the entry immediately above or below the entry is dated, MR may assume the date of the entry in question.
- Missing Signature
As much as possible, agencies should not add late signatures to the medical record, but should use the signature attestation process instead as Medicare does not accept retrospective orders. If a clinical diagnostic test order does not require a signature, regulations state that there must be medical documentation authenticated via a handwritten or electronic signature by the treating physician that they intended the clinical diagnostic test to be performed.
- Illegible Signature
Agencies may submit a signature log or attestation to support the identity of the signer, as contractors will be looking for some indication in other documentation to support the identity of the signer.
- Signature Log
A signature log is a typed listing of practitioner names with their handwritten signatures, which can be used to establish signature legibility. MR encourages practitioners to include their professional credentials and titles on the signature log.
- Signature Attestation
A signature attestation or attestation statement is used to authenticate an illegible or missing signature on medical documentation. For it to be valid, it must meet the following criteria:
- Signed and dated by the author of the medical record entry
- Have sufficient information to identify the beneficiary
- Reflect the printed full name of the physician or practitioner
- Reflect the date of service
Attestation statements are unacceptable when there is no associated medical record entry, or when they are from someone other than the author of the medical record entry.
- Signature for Amendments, Corrections, and Delayed Entries
Health record documents submitted containing amendments, corrections, or addenda must clearly and permanently be identified as such, clearly indicate the date and author of the entry, and identify all original content without deletion. Amendments or delayed entries may be initialed and dated if the medical record contains evidence associating the practitioner’s initials with their name. When correcting electronic health records, entries must provide a reliable means to identify the original content, the modified content, and the date and authorship of each modification of the record.
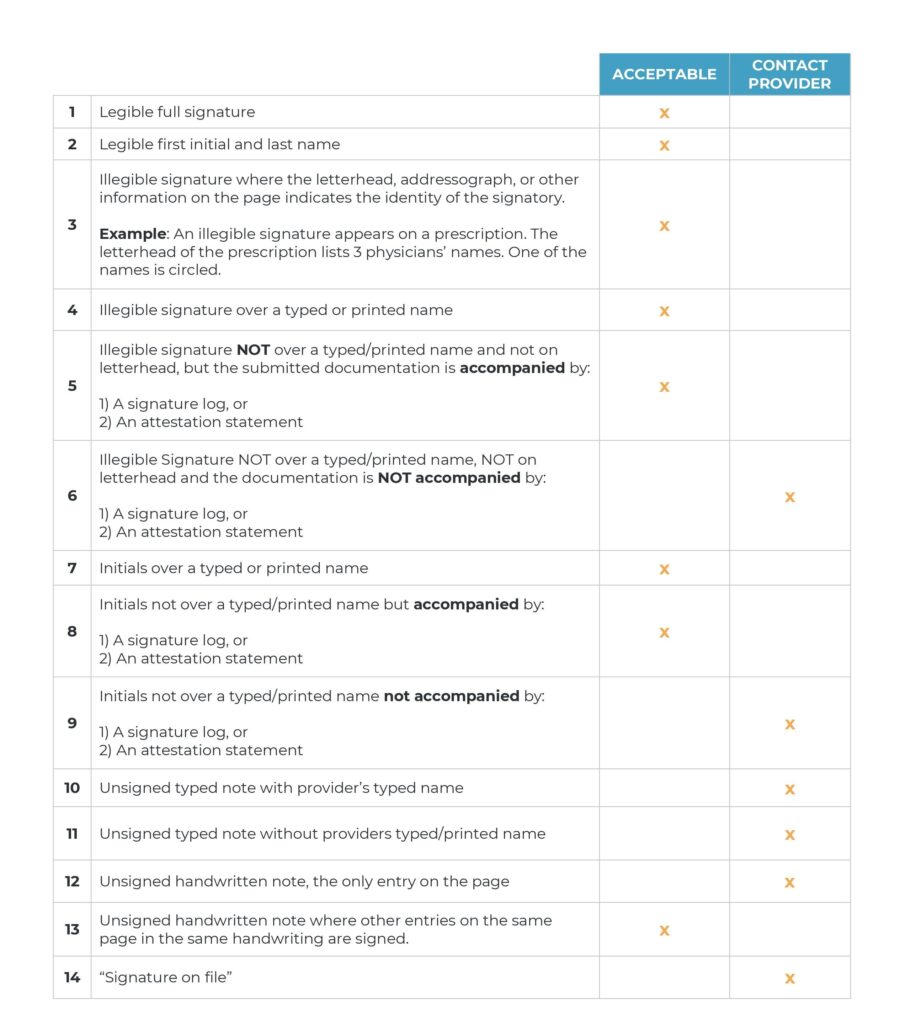
For further guidance, see table below:
Addressing the Challenges
As the first to handle the medical records from physicians or referral sources, the intake team should be well-trained to check the signatures. Moreover, they should also be able to immediately request an attestation when a signature does not meet the CMS standards. It would also help to ask your QA team or provider if they can include signature checking in their scope as well.
Another best practice is to keep a file of your agency’s e-signature policy, as well as a signature log of all clinicians and physicians/NPPs you are working with. This will be useful in case of additional development requests (ADRs) or surveys.
While letting the intake team check for signature compliance is good practice, it can also be challenging, considering the amount of documentation an agency handles, which usually involves manual sending, tracking, receiving, and checking of medical records.
To address this, take advantage of available tools and technology that can streamline your electronic medical records (EMR) management workflow. There are EMR integrations that can automatically send, track, receive, and upload medical records without human intervention, giving your intake team more time to focus on checking documents for compliance.
Aside from certifying the medical necessity of healthcare services, it is crucial for signatures to appear in acceptable formats. Reasons for ADRs and denial of claims are often linked to issues with practitioners’ signatures. While checking signatures may be tedious and time-consuming, it is an important task that can significantly reduce reimbursement issues.

